LET PATIENT FLOWS TELL YOU HOW WELL PRIMARY CARE IN YOUR REGION IS WORKING
- How important is a certain doctor for the functioning of primary care in a certain region
- How many and which doctors’ retirements can the system absorb?
- At what point can primary health care no longer be guaranteed for everyone?
Questions like these keep stakeholders in the health care system busy. They now can get help from the Hub. Our researchers developed a method to infer the resilience of a health care system in real time from its doctors’ networks. The paper just appeared in PNAS.
The innovative approach, a 1:1 computer model of the Austrian health care system, is based on data of patient flows between doctors in regional physician networks.
HOW SAFE IS THE PRIMARY HEALTH CARE SYSTEM?
Usually, the number of physicians in relation to the population—the so-called physician density—is used as an indicator for the quality of health care. Yet, this indicator assumes that all physicians are equally accessible and equally important for all patients. “We show that this is not the case,” says Peter Klimek.
“Physicians and their patients form networks. With the same physician density, these networks can either be resilient or prone to collapse, or something in between,” Peter points out.
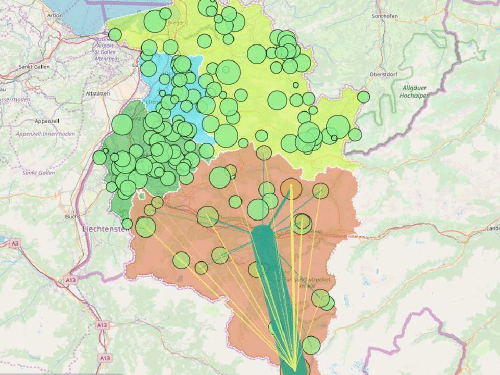
The Hub researchers used a research data set including all Austrian physicians and patient streams from 2006/2007 to create the network. Resident physicians are the nodes, connected to each other by their patients. “We were surprised at how closely connected and regionally focused the networks of patient flows are,” mentions Peter. They called this “patient sharing.”
This point becomes relevant as soon as a doctor’s office closes. The data show that more than 80 percent of all patients choose physicians for their further medical care with whom they have previously had contact. Knowing that, the researchers are able to calculate with high accuracy where patients of a particular doctor will turn after the doctor’s retirement.
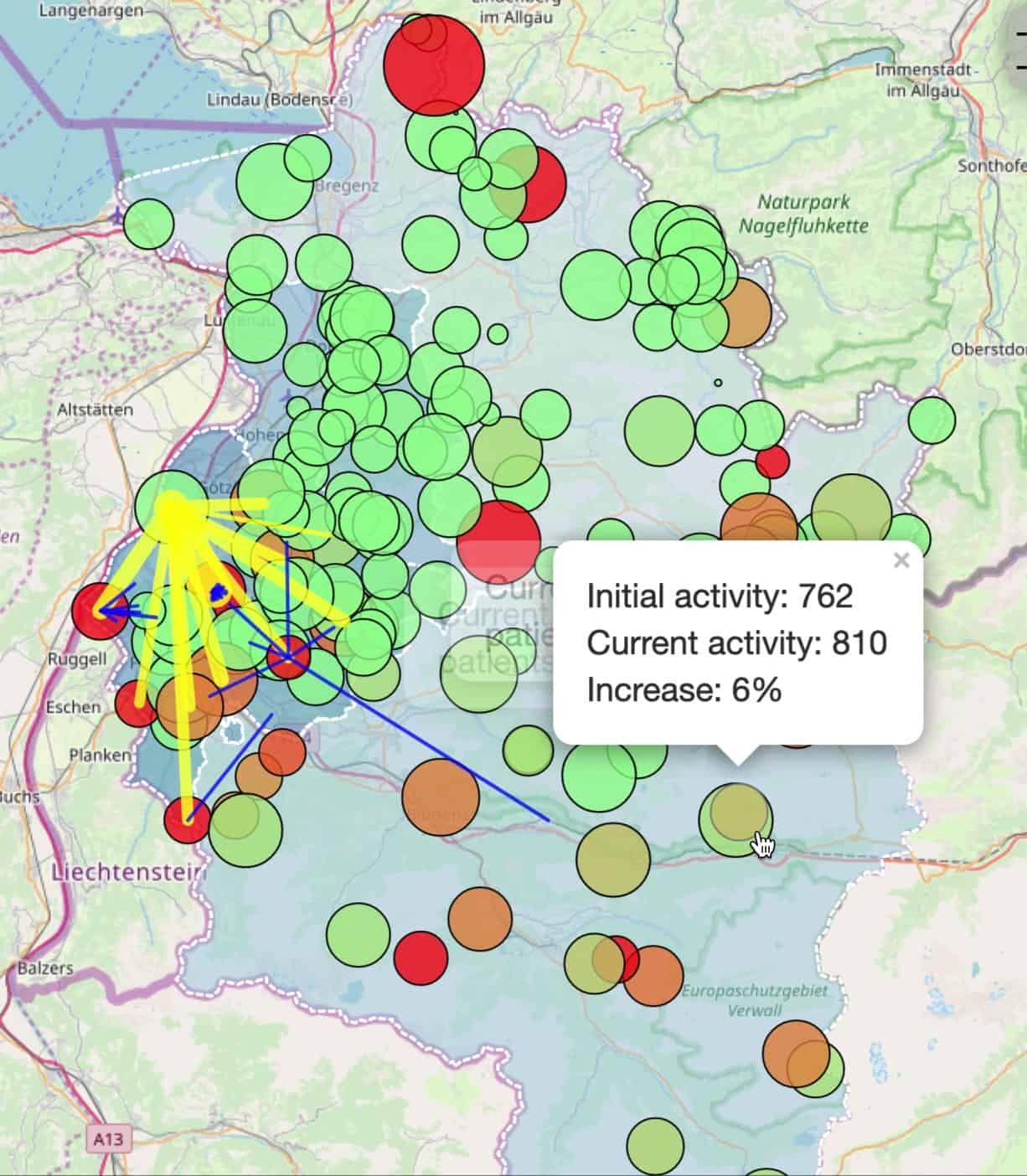
SIMULATION MAKES PATIENT FLOWS VISIBLE
An interactive simulation, programmed by Johannes Sorger, illustrates the network dynamics. In the simulation, natural persons of the Austrian province Vorarlberg were replaced 1:1 by anonymous avatars. “We can click away single doctor avatars and observe where their patients are moving on to,” explains Peter.
To try it yourself, just follow this link.
Or you watch this short screen recording.
HOW GOOD IS THE SYSTEM IN ABSORBING SHOCKS?
A resilient health care system will recover quickly and fully from such shocks. However, the loss of too many doctors at a time or of particularly important doctors can overstrain the system.
“The simulation shows the critical point at which the system’s ability to absorb additional patients or compensate for lost doctors collapses,” states the first author of the publication, Donald Ruggiero Lo Sardo (known as Ruggiero at the Hub). The present work was part of his PhD thesis.
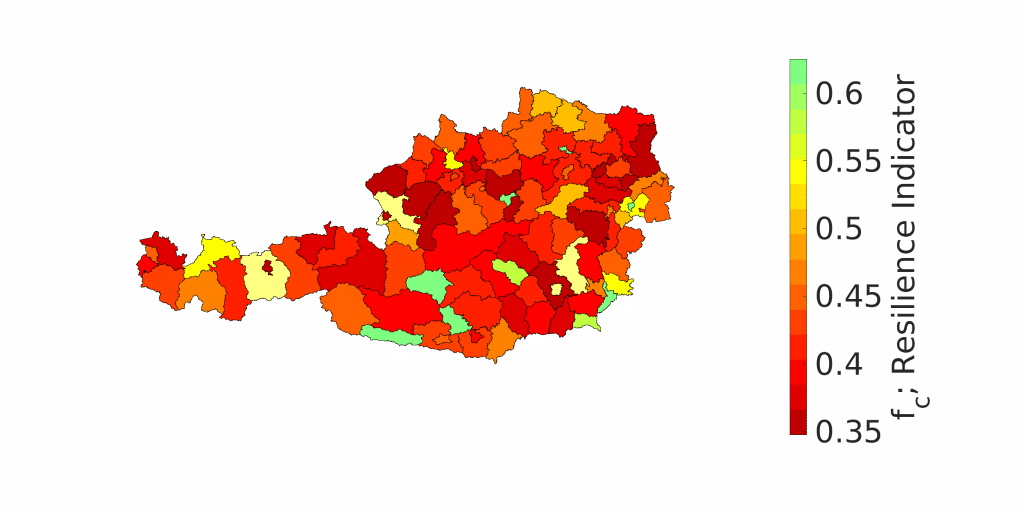
“Thanks to our model, we know how many and which doctors can be removed from the system without problems,” Ruggiero adds. “We can say how resilient the health care system is in a certain region. And we can determine how relevant each avatar is to the stability of the regional network.” For example, doctors with particularly large numbers of patients and good accessibility within the doctors’ network lend stability to the system. Poorly networked doctors, on the other hand, will more likely weaken the system.
A MODEL FOR MANY AREAS
The model provides stakeholders in the health care sector with a tool that allows (personnel) decisions and their effects to be tested in advance.
The researchers emphasize that the new method can be extended to diverse scenarios, such as the outbreak of an epidemic or a natural disaster with many casualties. “With up-to-date data, we can make valid assertions about the resilience of different sub-systems in health care,” maintains Peter. This knowledge facilitates planning and improves medical care. “As soon as people in charge know the systemically relevant doctors in a region, they can make the health care system more resilient by either trying to retain those doctors or to adequately refill their positions after their leave,” Peter concludes.
The paper, called “Quantification of the resilience of primary care networks by stress-testing the health-care system”, appears in the latest issue of the journal PNAS.
[CSH Press Release in English]
[Presseaussendung auf Deutsch]